Opioids, a class of powerful pain-relieving drugs, have seen a dramatic increase in prescription and abuse over the past two decades. While initially intended for pain management, their effects on mental health, particularly on individuals suffering from depression, have garnered significant attention. This article delves into how opioids affect those with depression, exploring both the potential short-term relief and the long-term consequences.
Understanding Opioids and Depression
Opioids: A Brief Overview
Opioids, including prescription medications like oxycodone and hydrocodone, as well as illegal substances like heroin, work by binding to opioid receptors in the brain and spinal cord, reducing the perception of pain. They also release dopamine, a neurotransmitter associated with pleasure, which can create a sense of euphoria.
Depression: A Complex Mental Health Condition
Depression is a common mental health disorder characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in activities. It can significantly impair an individual’s daily functioning and quality of life. The causes of depression are multifaceted, involving genetic, biological, environmental, and psychological factors.
Short-Term Effects of Opioids on Depression
Initial Euphoria and Relief
For individuals suffering from depression, the initial use of opioids can provide temporary relief. The euphoric effects of opioids can momentarily lift their mood, reduce anxiety, and create a sense of well-being. This initial phase can be deceptive, as the pleasure derived from opioid use may lead individuals to believe that these drugs are beneficial for their mental health.
Temporary Pain Alleviation
Depression often coexists with chronic pain conditions. Opioids’ pain-relieving properties can also alleviate physical discomfort, which might indirectly improve mood and overall sense of well-being in the short term.
Long-Term Consequences of Opioid Use on Depression
Development of Tolerance and Dependence
With prolonged use, individuals develop tolerance to opioids, requiring higher doses to achieve the same effects. This can lead to physical and psychological dependence, where the individual feels unable to function normally without the drug. Dependence often exacerbates depression symptoms, creating a vicious cycle of use and withdrawal.
Worsening of Depression Symptoms
Studies have shown that long-term opioid use can worsen depression. The initial euphoria diminishes, and individuals may experience heightened anxiety, irritability, and depressive symptoms during withdrawal periods. This can lead to increased use of opioids in an attempt to stave off these negative feelings, further deepening the dependence.
Impact on Neurotransmitter Systems
Opioids affect the brain’s neurotransmitter systems, particularly those involving dopamine and serotonin. Chronic use can disrupt these systems, leading to a decrease in the brain’s natural ability to produce these chemicals. This disruption can result in a heightened state of depression once the effects of the opioids wear off.
The Risk of Co-occurring Disorders
Dual Diagnosis
Many individuals with depression who misuse opioids may be diagnosed with co-occurring disorders or dual diagnosis. This refers to the simultaneous presence of a substance use disorder and a mental health disorder. Dual diagnosis complicates treatment, as both conditions need to be addressed concurrently for effective recovery.
Increased Risk of Suicide
The combination of depression and opioid use significantly increases the risk of suicide. The disinhibition caused by opioid intoxication, coupled with the severe lows experienced during withdrawal, can lead individuals to act on suicidal thoughts.
Treatment and Recovery
Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) is a comprehensive approach to treating opioid use disorder that combines the use of medication with counseling and behavioral therapies. MAT has proven effective in helping individuals achieve and maintain recovery, while also addressing the symptoms of depression.
Medications Used in MAT
– Methadone: A long-acting opioid agonist that reduces cravings and withdrawal symptoms without producing the euphoria associated with opioid misuse.
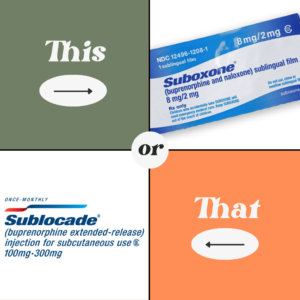
– Buprenorphine: A partial opioid agonist that helps to alleviate withdrawal symptoms and reduce cravings, while also having a ceiling effect that lowers the risk of misuse.
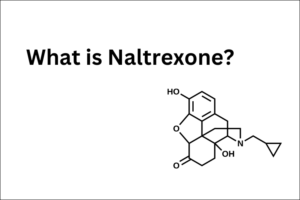
– Naltrexone: An opioid antagonist that blocks the euphoric and sedative effects of opioids, helping to prevent relapse. Naltrexone is also available in an extended-release injectable form, making it easier for patients to adhere to treatment.
Benefits of MAT
– Stabilization of Mood: By managing withdrawal symptoms and reducing cravings, MAT helps to stabilize the mood of individuals with opioid dependence, which can, in turn, alleviate some symptoms of depression.
– Improved Retention in Treatment: The use of medication can make it easier for individuals to remain in treatment programs, improving their chances of long-term recovery.
– Enhanced Functioning: MAT can improve overall functioning, allowing individuals to better engage in therapy and other recovery activities.
Psychotherapy
Cognitive-behavioral therapy (CBT) and other forms of psychotherapy can help individuals develop coping strategies, address underlying issues, and manage depressive symptoms. Therapy can provide the tools necessary to navigate the challenges of recovery and build a healthier, more fulfilling life.
Support Groups
Participation in support groups like Narcotics Anonymous (NA) and depression support groups can provide social support and shared experiences. These groups offer a sense of community and understanding, which can be invaluable during the recovery process.
Holistic Approaches
Incorporating holistic approaches, such as exercise, nutrition, mindfulness practices, and alternative therapies, can support overall mental and physical health, aiding in recovery from both depression and opioid dependence.
Conclusion
While opioids may offer short-term relief for individuals suffering from depression, their long-term use can lead to devastating consequences, including worsening depression, development of dependence, and increased risk of suicide. Integrated treatment approaches, particularly Medication-Assisted Treatment, that address both opioid dependence and depression are essential for effective recovery. Understanding the complex relationship between these two conditions is crucial for healthcare providers, patients, and their families in navigating the path to healing.
FAQs
What are the short-term effects of opioids on depression?
The short-term effects of opioids on depression include initial euphoria, temporary mood lift, and relief from chronic pain, which can momentarily improve the overall sense of well-being.
How do opioids worsen depression in the long term?
Opioids worsen depression in the long term by creating tolerance and dependence, disrupting neurotransmitter systems, and leading to increased anxiety and depressive symptoms during withdrawal periods.
What is dual diagnosis?
Dual diagnosis refers to the simultaneous presence of a substance use disorder and a mental health disorder, such as depression. This complicates treatment as both conditions need to be addressed concurrently.
How does Medication-Assisted Treatment (MAT) help with opioid dependence and depression?
MAT helps by using medications to manage withdrawal symptoms and reduce cravings, stabilizing mood, improving retention in treatment programs, and enhancing overall functioning to support recovery from both opioid dependence and depression.
Why is psychotherapy important in treating depression and opioid dependence?
Psychotherapy, such as cognitive-behavioral therapy (CBT), helps individuals develop coping strategies, address underlying issues, and manage depressive symptoms, providing essential tools for navigating recovery.
What role do support groups play in recovery from opioid dependence and depression?
Support groups offer social support, shared experiences, and a sense of community, which are invaluable for individuals recovering from opioid dependence and depression. They provide understanding and encouragement throughout the recovery process.