In the journey to overcome opioid addiction, understanding the tools available for recovery is crucial. Suboxone, a medication specifically designed to ease withdrawal symptoms and reduce cravings in opioid-dependent individuals, plays a pivotal role in this process. However, when addiction coincides with mental health disorders—a situation known as dual diagnosis—the path to recovery can become more complex but not insurmountable. This blog post delves into the intricate relationship between dual diagnosis and Suboxone treatment, offering insights into how this medication can be a cornerstone of successful recovery strategies.
Understanding Dual Diagnosis
Dual diagnosis occurs when someone faces both a substance use disorder, like opioid addiction, and a mental health condition such as depression or anxiety. Recognizing both issues is crucial because they often affect each other. For instance, mental health problems can lead to drug use as a way of coping, while substance abuse can worsen mental health conditions.
Treatment for dual diagnosis can be challenging because it involves addressing both the addiction and the mental health issue simultaneously. However, understanding this complexity is the first step toward effective management and recovery.
The Role of Suboxone Treatment for Dual Diagnosis
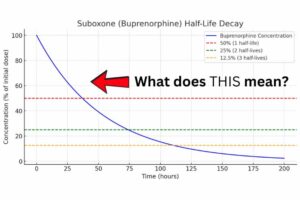
Suboxone is a medication that combines buprenorphine and naloxone. It is primarily used to treat opioid addiction, helping to reduce cravings and withdrawal symptoms. For individuals with dual diagnosis, Suboxone offers several key benefits:
- Managing Withdrawal: Suboxone helps alleviate the discomfort of opioid withdrawal, which can be particularly intense for those dealing with co-occurring mental health issues.
- Reducing Cravings: By mitigating cravings, Suboxone allows individuals to focus more on therapy and recovery strategies for both their addiction and mental health issues.
- Safety Features: The inclusion of naloxone in Suboxone acts as a safeguard against misuse, as it can block the effects of opioids and precipitate withdrawal symptoms if the medication is not used as prescribed.
Effective use of Suboxone in dual diagnosis treatment requires careful monitoring and adjustment by healthcare providers. It’s a cornerstone for building a stable platform from which patients can engage in other therapeutic interventions essential for treating their co-occurring mental health disorders.
Challenges in Dual Diagnosis Treatment
Treating dual diagnosis involves unique challenges that complicate the recovery process. Here are some key obstacles:
- Complex Diagnosis: It can be difficult to diagnose co-occurring disorders accurately because symptoms of substance abuse and mental health issues often overlap. Misdiagnosis or overlooking one condition can hinder effective treatment.
- Integrated Treatment Requirement: Dual diagnosis requires a coordinated approach that combines mental health services and substance abuse treatments. However, finding treatment programs that offer integrated services tailored to individual needs can be challenging.
- Higher Relapse Risk: Individuals with dual diagnosis have a higher risk of relapse because mental health disorders can trigger substance use as a coping mechanism. This interplay demands continuous monitoring and adaptation of treatment plans.
- Social Stigma and Isolation: The stigma surrounding mental health issues and addiction can lead to social isolation, making it harder for individuals to seek help and sustain recovery.
- Resource Availability: Access to comprehensive dual diagnosis programs is often limited, especially in rural or underserved areas. This can delay or prevent individuals from receiving the appropriate care they need.
Effective Strategies for Dual Diagnosis Treatment
Successfully managing dual diagnosis requires an integrated, multifaceted approach. Here are several strategies that have proven effective:
- Integrated Treatment Programs: Combining mental health and addiction treatment services under one program allows for a more holistic approach. This ensures that both aspects of dual diagnosis are treated simultaneously, which can improve outcomes and reduce the likelihood of relapse.
- Personalized Care Plans: Each individual’s circumstances are unique, requiring customized treatment plans that address specific mental health issues along with addiction. Tailored therapies can include combinations of medication-assisted treatment, psychotherapy, and support groups.
- Continuous Support and Monitoring: Long-term success in dual diagnosis treatment often depends on continuous support and regular monitoring. This includes ongoing counseling, support groups, and sometimes case management services to help individuals navigate the complexities of their treatment and recovery.
- Education and Awareness: Educating patients and their families about dual diagnosis can empower them, reduce stigma, and enhance the effectiveness of treatment. Understanding the nature of the disorders and the rationale behind treatment choices fosters a cooperative relationship between patients and healthcare providers.
- Access to Resources: Providing access to additional resources, such as housing, employment assistance, and educational opportunities, can support the recovery process. These resources help to stabilize the lives of individuals in recovery, making it easier to focus on maintaining their mental health and sobriety.
Common Outcomes in Dual Diagnosis Treatment
Discussing the typical outcomes observed in dual diagnosis treatment can provide a realistic perspective on what individuals and their families might expect. Here are some commonly observed outcomes from integrated treatment programs:
- Improved Management of Symptoms: Patients often report better management of both mental health symptoms and addiction-related behaviors as a result of integrated treatment approaches. This includes reduced cravings and a better ability to handle stress and emotional triggers.
- Enhanced Quality of Life: Many individuals experience a significant improvement in their overall quality of life, including better relationships, increased job stability, and a return to hobbies and activities they enjoy. These improvements are crucial for long-term recovery and personal fulfillment.
- Increased Treatment Adherence: Programs that offer coordinated care for dual diagnosis tend to see higher rates of treatment adherence. Patients are more likely to stay engaged with treatment when their mental health and substance use disorders are addressed simultaneously.
- Reduction in Relapse Rates: While relapses can be a part of the recovery journey, integrated treatment programs often report lower relapse rates. This success is attributed to the comprehensive nature of care, which equips individuals with the tools to manage both sets of conditions effectively.
- Greater Resilience: Over time, patients develop greater resilience against the challenges posed by their conditions. Learning and applying new coping strategies are key components of treatment that contribute to this resilience.
Conclusion
As we’ve explored throughout this post, dual diagnosis—where an individual confronts both a mental health condition and substance use disorder—requires a nuanced and integrated treatment approach. Suboxone, combined with comprehensive therapy and support systems, plays a crucial role in managing symptoms and fostering long-term recovery. The common outcomes of improved symptom management, enhanced quality of life, higher treatment adherence, reduced relapse rates, and increased resilience underscore the effectiveness of integrated treatment programs.
Recovery from dual diagnosis is a journey, one that is both challenging and rewarding. For those struggling with these complex conditions, or their loved ones seeking to support them, knowing that there are effective treatments available that offer hope and a path forward is essential. With the right support and a tailored treatment plan, recovery is not just a possibility, but an achievable goal.
We encourage anyone dealing with these issues to reach out for help and to remember that with the right treatment and support, a healthier, more stable life is within reach. For more information or to find support services near you, consult healthcare providers who specialize in addiction and mental health.