When considering treatment options for opioid use disorder (OUD), many patients and healthcare providers explore the benefits of switching from Suboxone to Sublocade. Both medications play a role in Medication-Assisted Treatment (MAT), effectively reducing cravings and managing withdrawal symptoms. However, the idea of using Sublocade and Suboxone together raises questions about safety, effectiveness, and appropriate use. Understanding the key differences between these two options is crucial for choosing the right treatment plan.
Suboxone combines buprenorphine, a partial opioid agonist, with naloxone, an opioid antagonist that deters misuse. Patients typically take it as a sublingual film or tablet once daily, making it suitable for at-home use.
Sublocade is an extended-release injection containing only buprenorphine. Administered once a month by a healthcare professional, it provides a steady release of medication over time. This method can be more convenient for patients who prefer not to take medication daily.
Understanding these differences is crucial for choosing the right treatment plan.
Breaking Down the Basics: Understanding Suboxone vs Sublocade
To decide between Suboxone and Sublocade, understanding their basic components and how each works to treat OUD is important.
Suboxone Composition and Use: Suboxone contains buprenorphine, which reduces cravings and withdrawal symptoms without causing a strong high. It also includes naloxone to prevent misuse. If someone injects Suboxone rather than taking it orally, naloxone triggers immediate withdrawal symptoms, deterring potential abuse.
Sublocade Composition and Use: Sublocade, on the other hand, is a long-acting formulation of buprenorphine without naloxone. It is designed for patients who have stabilized on a daily buprenorphine regimen and prefer less frequent dosing. A healthcare provider gives Sublocade as a monthly injection. The injection slowly releases buprenorphine over time, helping maintain stable medication levels and reducing the risk of relapse.
Both medications bind to opioid receptors in the brain, but their methods of administration and formulations make them distinct choices depending on patient needs and treatment goals.
A Closer Look: Suboxone vs Sublocade for Opioid Addiction
Both Suboxone and Sublocade effectively treat opioid addiction, but they offer different benefits depending on the patient’s circumstances.
Effectiveness: Suboxone has been widely used for many years and effectively reduces opioid misuse when taken as directed. It is particularly useful for patients who need a flexible treatment option that allows for daily, at-home administration.
Patient Convenience: Sublocade may be a better option for patients who find it challenging to adhere to a daily medication regimen. The once-monthly injection ensures steady medication levels. This method may also reduce the temptation to misuse the drug since healthcare providers handle its administration.
Potential for Misuse: Suboxone’s inclusion of naloxone specifically prevents misuse, making it a safer option for some patients. Meanwhile, Sublocade’s injectable format significantly reduces the risk of misuse compared to medications taken at home.
The choice between Suboxone and Sublocade should involve consultation with a healthcare provider, considering factors like patient lifestyle, risk of misuse, and personal preferences.
Suboxone vs Sublocade: A Closer Look at the Benefits and Drawbacks
Each medication has its own benefits and drawbacks that must be weighed when deciding on a treatment plan.
Benefits of Suboxone:
- Flexibility: The ability to take medication at home provides flexibility for patients with busy or unpredictable schedules.
- Safety Profile: The inclusion of naloxone helps prevent misuse, making it a safer choice for patients at risk of misusing the medication.
Drawbacks of Suboxone:
- Daily Dosing Requirement: The need to take the medication daily can burden some patients, leading to inconsistent adherence.
- Potential for Misuse: Despite the inclusion of naloxone, there is still a risk of misuse if the medication is not taken as prescribed.
Benefits of Sublocade:
- Reduced Risk of Diversion: Administered in a clinical setting, Sublocade significantly reduces the risk of diversion or misuse.
- Convenience: The monthly injection eliminates the need for daily medication, which can enhance adherence and reduce the stigma associated with daily opioid treatment.
Drawbacks of Sublocade:
- Accessibility and Cost: Sublocade may be more expensive and less accessible than Suboxone. It requires administration by a healthcare provider and may not be covered by all insurance plans.
- Injection Site Reactions: Some patients may experience pain or discomfort at the injection site. This could be a drawback for those sensitive to injections.
Overall, both Suboxone and Sublocade are effective treatment options for OUD. The decision between them should be tailored to each patient’s specific needs and circumstances.
Is Switching Safe and Effective?
Switching from Suboxone to Sublocade in Medication-Assisted Treatment (MAT) for opioid use disorder (OUD) can better align treatment with a patient’s needs and lifestyle. Both medications contain buprenorphine, but they offer different benefits. Each may be more suitable at different stages of recovery or for different patient preferences. Understanding when and how to switch between these medications safely is crucial for maintaining effective treatment and avoiding withdrawal symptoms.
Common Questions About Switching
Can I switch from Suboxone to Sublocade safely?
Yes, switching from Suboxone to Sublocade is generally safe when conducted under a healthcare provider’s guidance. The switch typically involves stabilizing on Suboxone first to ensure that the patient can tolerate buprenorphine. Once stabilized, the provider administers Sublocade as a monthly injection. This method helps reduce the risk of withdrawal symptoms and ensures a smooth transition.
Why might someone switch from Suboxone to Sublocade?
There are several reasons why a patient might switch from Suboxone to Sublocade:
- Convenience: Sublocade requires only a once-monthly injection, which can be more convenient than taking Suboxone daily. This reduces the burden of daily medication management and can help improve adherence.
- Reduced Risk of Misuse: Because Sublocade is administered by a healthcare provider, there is less risk of misuse or diversion compared to Suboxone, which is taken at home.
- Stable Medication Levels: Sublocade provides a steady release of buprenorphine over a month, which can help maintain consistent therapeutic levels and potentially reduce the risk of relapse.
Is it possible to switch back from Sublocade to Suboxone?
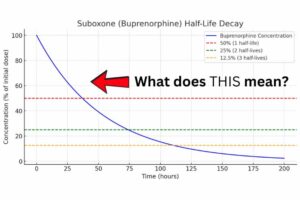
Yes, switching from Sublocade back to Suboxone is possible, but it requires careful planning to avoid withdrawal symptoms. Because Sublocade is an extended-release formulation, it is essential to wait until the medication has sufficiently metabolized before starting Suboxone. The healthcare provider will guide this process, ensuring the switch is timed correctly and that the patient is closely monitored.
How to Transition from Suboxone to Sublocade
Making the switch from Suboxone to Sublocade involves several steps to ensure a safe and effective transition:
- Consult with Your Healthcare Provider: Discuss your options with your healthcare provider before making any changes. They will assess your current treatment plan and medical history to determine if switching to Sublocade is appropriate for you.
- Stabilize on Suboxone: You will need to stabilize on a daily Suboxone regimen for at least seven days. This step ensures that your body is accustomed to buprenorphine, reducing the likelihood of withdrawal symptoms when transitioning to Sublocade.
- Receive the First Sublocade Injection: After stabilization, your healthcare provider will administer the first Sublocade injection. This injection is given under the skin and releases buprenorphine gradually over the month. The initial dosage will be carefully monitored to observe any immediate reactions or side effects.
- Follow-Up and Monitor: Regular follow-up appointments are crucial after receiving the Sublocade injection. Your provider will monitor your response to the medication and make any necessary adjustments to your treatment plan. They will also check for any signs of withdrawal or side effects.
By following these steps, patients can transition from Suboxone to Sublocade smoothly, ensuring continued support in their recovery journey.
How to Transition from Sublocade to Suboxone
Switching from Sublocade back to Suboxone may be necessary for some patients due to personal preferences, lifestyle changes, or side effects experienced with Sublocade. Here’s a step-by-step guide to help manage this transition:
- Discuss with Your Healthcare Provider: If you’re considering switching back to Suboxone, your healthcare provider will help determine the best timing for the switch. They will evaluate how long it has been since your last Sublocade injection and assess any withdrawal symptoms.
- Wait for Sublocade to Metabolize: Given that Sublocade is a long-acting injection, it’s important to wait until the buprenorphine has sufficiently metabolized to avoid overdose or severe withdrawal symptoms. Your provider will advise you on the appropriate wait time based on your last injection.
- Start with a Low Dose of Suboxone: Once it’s safe to begin Suboxone, your healthcare provider will start you on a lower dose. This cautious approach helps minimize the risk of withdrawal and allows for gradual adjustment to the daily dosing routine.
- Adjust Dosage as Needed: As you transition to Suboxone, your provider may adjust your dose based on your response. Close monitoring will help ensure that your treatment remains effective and that any side